Study Finds 21% of Serious
Eye
Injuries Due to LASIK!
Thirty-one months after it
back-burnered a former CDRH branch chief’s petition seeking withdrawal of the
LASIK indication for ophthalmic lasers based on unacceptably high permanent
injury rates, CDRH has been sent a new retrospective study indicating that 21%
of patients with serious corneal pain had received laser surgery on their eyes.
The 6/14 study, from Harvard Medical School assistant clinical professor and
Boston EyePain Foundation founder Perry Rosenthal, found 21 out of 100
consecutive patients diagnosed with centralized corneal pain had previously
undergone laser keratorefractive surgery.
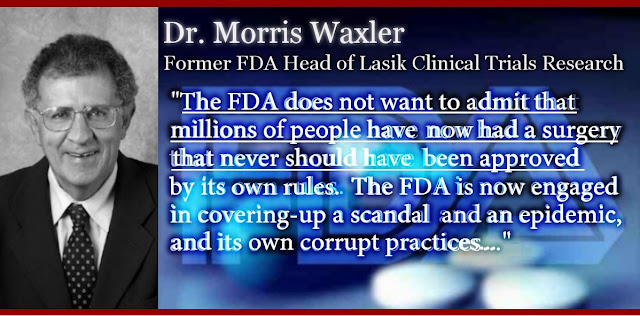
In his moribund petition, former
CDRH branch chief for diagnostic and surgical devices Morris Waxler complained
about a LASIK industry-promoted injury rate of less than 1% on which his review
team had based its approval of the devices, compared with his subsequent
assessment of an injury rate in excess of 20%. Waxler alleged that
“Manufacturers and their collaborators withheld more than 10% of the adverse
event data from 13 of the 25 studies, more than 20% from 12 studies, and more
than 40% from seven studies.”
The new study by Rosenthal,
which was rejected by two ophthalmic professional journals* heavily supported
by the LASIK industry, carries the adverse event rate far beyond the six-month
post-operative followup point in most of Waxler’s data, extending out as far as
15 years post-op. Rosenthal found eight patients who had experienced symptoms
immediately after surgery, three whose symptoms were delayed between three and
28 days, two who experience symptoms between one and six weeks post-op, and
eight whose symptoms began between one and 15 years post-op.
Rosenthal’s study describes the
symptoms observed as chronic centralized neuropathic corneal pain. It says the
recognition that this “can be a complication of laser keratorefractive surgery
is the first step to developing mechanism-based treatments for this overlooked,
crippling and currently intractable neurological complication.”
Rosenthal acknowledges in the
study that the 21 subjects described differed from those who experienced
“typical” post-LASIK dry eye-like pain in that they reported “higher intensity
descriptors such as burning, aching, pressure, stabbing and in many of these
patients, the presence of otherwise unexplainable photosensitivity
(photoallodnia).”
He dismisses what he calls
“anecdotal observations” that suggest centralized corneal neuropathic pain is
rare. “This begs the question of why some people are susceptible to this
complication,” he writes. “Vulnerability to neuropathic pain is believed to be
influenced by certain genetic and epigenetic factors and efforts to develop
useful predictive tests continue, including measurements of an individual’s
endogenous sensitivity to pain.”
Rosenthal recommends screening
of LASIK candidates for family history of autoimmune diseases which are known
to be associated with a higher incidence of peripheral neuropathies. “Reports
that delayed treatment of post-operative pain has a deleterious effect on pain
outcomes suggest that [post LASIK] pain should be treated aggressively and
perhaps even preemptively,” Rosenthal says in his study report. “In this
context, early interventions that accelerate corneal epithelial and nerve
healing and suppress inflammation may also be helpful in avoiding the
transition to centralized corneal neuropathic pain. Because of thedevastating
nature of this complication the search for effective topical analgesics capable
of being used safely prior to and for an extended period of time after surgery
is, in my opinion, a high priority.”
* Elsevier’s Journal of the
American Academy of Ophthalmology and The Journal of Cataract and Refractive
Surgery


No comments:
Post a Comment